Whether it’s work pressure, family demands, or the general curveballs life enjoys throwing our way, stress and pain have become unwelcome companions for many people. They’re tough enough on their own — but throw an acute, cumulative, or chronic injury into the mix, and things can get complicated fast.
But have you ever stopped to wonder which one actually kicks things off?
Does stress cause pain?
Does pain cause stress?
Or are they just terrible roommates who constantly make each other worse?
In this blog post, I’ll dig into the intricate relationship between stress and pain, explore the science behind their connection, and look at practical strategies to help break the cycle.
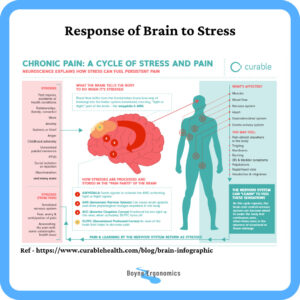
How The Brain Reacts To Stress
Here’s the simple version — no neuroscience degree required.
When we feel threatened, overwhelmed, or under pressure, the brain hits the “all hands on deck” button. Blood flow shifts away from the frontal lobes — the part responsible for logic, planning, calm decisions — and into the limbic system, our emotional command centre.
A few key players jump into action:
• Dorsolateral Prefrontal Cortex (DPC)
This area helps regulate pain. Under stress? It powers down. Not ideal.
• Amygdala
The alarm bell. It fires up the Autonomic Nervous System (fight/flight/freeze) and primes the body for action, not comfort.
• Anterior Cingulate Cortex (ACC)
This one manages emotion, impulse control, and decision-making. When it ramps up, the DPC switches off — again reducing the brain’s natural ability to dampen pain.
This cascade can influence pretty much every major system:
- Musculoskeletal (hello tense shoulders)
- Circulatory
- Nervous
- Gastrointestinal
- Genito-urinary
When people say “stress is physical,” they’re not kidding.
The Stress-Pain Connection
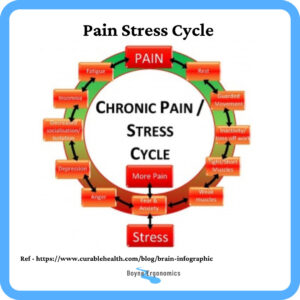
Stress and pain are closely interconnected due to the complex relationship between the mind and body. The brain plays a pivotal role in this connection, as it processes both emotional and physical experiences.
Stress triggers the body’s “fight or flight” response, releasing hormones like cortisol and adrenaline. These hormones can lead to muscle tension, increased heart rate, and heightened sensitivity to pain. In DSE based workers, this response can often be felt as a tightness across the shoulders and into the neck as this is where a lot of people carry their stress and anxiety.
Furthermore, chronic stress can disrupt the body’s natural pain modulation systems, making it more difficult to manage and alleviate pain. The brain’s focus on stress-related thoughts can amplify pain perception, leading to a vicious cycle where stress worsens pain and pain, in turn, heightens stress levels.
Now consider the impact an injury can have on levels of stress. If a person develops pain or suffers an acute injury, they may feel worried or anxious about the injury, how the injury might negatively affect their ability to work or to carry out day to day tasks. It may impact their quality of life. They may be worried about the financial implications of being out of work or affording appropriate treatment. It may impact their sleep and social relationships. Any of these factors can lead to an increase in the levels of stress a person experiences.
Some injuries result in decreased physical activity and mobility and this in turn can impact feelings of stress and pain.
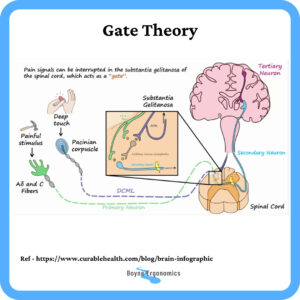
The Gate Control Theory
The Gate Control Theory, proposed by Melzack and Wall in 1965, describes a mechanism in the spinal cord that sends pain signals to the brain and influences how “severely” the pain is perceived. The perception of the pain is not equal to the intensity of the pain stimulus.
According to this theory, pain perception is influenced by both physical and psychological factors.
When stress or emotional distress occurs it can “open the gate” for pain signals to be intensified.
On the other hand, positive emotions and relaxation techniques can help “close the gate,” reducing the brain’s interpretation of pain signals. This theory can help explain why we rub or massage an area after we injure it, as it can activate the gate control mechanism, closing it, reducing the perception of the pain.
For any of you that have used a TENS machine for pain relief, this theory explains how it works too!
Breaking Down the Cycle
It’s important to recognize that the stress-pain cycle can vary from person to person. For some individuals, stress may indeed precede the experience of physical pain. For others, an underlying medical condition might lead to pain, which subsequently triggers stress and emotional distress. Regardless of the initial trigger, the continuous interaction between stress and pain can create a cycle that’s challenging to break.
Managing Stress and Pain Together
Before applying techniques to reduce the perception of stress and pain, my first recommendation is to try and identify the source of the issue.
If you are experiencing excessive stress and anxiety, try and identify the reasons and assess if any of these can be addressed. For example, if you find that you are stressed and anxious when at work, or even thinking about work tasks, why is this so? Is it the workload, the environment, the people, do you need more support or training? Seek professional assistance if you feel that this is not something you can work through on your own.
When it comes to pain and discomfort, seek medical attention as early as possible and work with your treating specialist to identify a cause. If you experience pain and discomfort in the workplace, advise your manager and request assistance to address the issues there, e.g an ergonomic risk assessment.
Below are five general tips to help manage your stress and or pain, to reduce the impact they have on each other and on your quality of life.
- Mindfulness and Meditation: Mindfulness techniques can help break the stress-pain cycle by promoting present-moment awareness. They can help you focus on the now, reducing worrying about the future. Meditation and deep breathing exercises can calm the mind, reduce stress hormones, and alleviate pain perception.
- Physical Activity: Regular exercise releases endorphins, which are natural pain relievers and mood enhancers. Engaging in physical activity can help manage stress and pain simultaneously. Make sure it is something you enjoy, even a short walk outside in fresh air can do wonders!
- Cognitive Behavioral Therapy (CBT): CBT is effective in managing both stress and chronic pain. It helps individuals identify and modify negative thought patterns that contribute to stress and pain amplification.
- Social Support: Talking about your experiences with friends, family or support groups can alleviate emotional distress and help in managing pain.
- Professional Help: Consulting healthcare professionals, such as doctors, physical therapists, or psychologists, can provide tailored guidance and treatments for managing stress and pain.
Conclusion
The question of what comes first, stress or pain, doesn’t have a simple answer. We all experience and respond to stressors and pain stimuli differently. The relationship between these two experiences is complex and bidirectional.
What I can say following research into this area, is that if you are experiencing stress or anxiety, this can exacerbate symptoms of underlying medical conditions and injuries. It can also lead to feelings of pain and discomfort in the absence of known pre-existing issues. Equally, based on individual circumstances, experiencing an injury, illness or discomfort can lead to stress or anxiety.
Understanding the science behind this connection empowers us to take proactive steps in managing both stress and pain effectively.
By identifying and addressing the source of the stress, anxiety, physical discomfort or pain, incorporating mindfulness, exercise, therapy, social support, and professional guidance, we can break the cycle and improve our overall well-being.
Remember, addressing stress and pain as a holistic duo is key to finding relief and achieving a higher quality of life.
Sources:
https://www.physio-pedia.com/Gate_Control_Theory_of_Pain
https://neuroscientificallychallenged.com
https://www.curablehealth.com/blog/brain-infographic
Melzack, R & Wall, P.D. (1965) Pain mechanisms: A new theory. Science. Nov 19;150(3699):971-9
Image ref PathoPhysioPharamco via YouTubethis blo

